Over the next few weeks, I am going to look at the impact that temporomandibular joint dysfunction (TMJD) can have on the physical & physiological wellbeing of an athlete, as well as the management strategies that can be used to treat it.
I will discuss the relationship & potential effect that TMJD may, or may not, have on aspects of performance development, execution, or recovery as unexpected & varied as skill acquisition, neuromuscular pathway refinement, concussion & collagen structure.
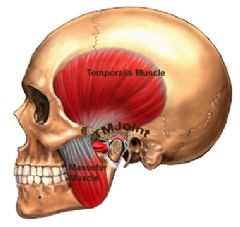
In the first instance, however, it is important to look at the basic anatomy of the temporomandibular joint (TMJ), it’s articular actions in addition to both its direct & indirect interfaces with the spine. This will lead primarily in to the influences that TMJD can have on balance, proprioception & biomechanics, which we will cover today.
The name ‘temporomandibular joint”, is considered by some to be more accurately termed the “craniomandibular joint”, given the anatomical nature of the structure. In either case, the joint is actually two joints, or a biarthrodal joint, consisting of two atypical ellipsoid synovial joints.
On either side, the joints are the articulations between the condyles of the mandible (jaw bone) & the squamous portion of the temporal bone. The condyles are elliptically-shaped with the long axes orientated mediolaterally.
The articular surface of the temporal bone consists of the concave articular fossa & the convex articular eminence. Attached to the articular eminence & surrounding the joint, is a fibrous membrane, which forms the joint capsule, further attaching to the articular disc (also called the meniscus) & neck of the mandibular condyle.
Being synovial in nature, the joint is filled with fluid & houses the body of the articular disc. The disc is a fibrous, saddle-shaped structure, which separates the condyle & temporal bone.
The disc attaches to the condyles both medially & laterality the collateral ligaments. Meanwhile, anteriorly, the disc attaches to the joint capsule & superior head of the lateral pterygoid. Posteriorly, the disc becomes more vascular & innervated as it transitions to the bilaminar zone, blending with the connective tissue that forms the attachment to the mandibular fossa.
The joint is supplied by the mandibular branch of the trigeminal nerve & the local effects of TMJD can be experienced by entrapment of the vagus, hypoglossal & trigeminal nerves. It is the impact on the trigeminal nerve that will be the focus of some of the discussions related to glial cell activation & collagen structure in this series.
Passive stability to the joint is provided by the ligamentous structures:
- Temporomandibular Ligament - thickened lateral capsular portion, consisting of the outer oblique fibres & the inner horizontal fibres
- Stylomandibular Ligament - originating at the styloid process & inserting in to the angle of the mandible
- Sphenomandibular Ligament - attaching along the spine of the sphenoid bone & then to the surface of the mandible
- Oto-mandibular Ligaments - firstly, the discomalleolar ligament, which originates from the malleus of the inner ear, attaching to the postero-medial portion of the disc & secondly the anterior malleolar ligament, which arises from the malleus & inserts into the sphenomandibular ligament so as to connect with the surface of the mandible.
These latter two ligaments are important considerations when relating TMJD to balance & proprioceptive problems in athletes. This is because TMJD may stretch these two ligaments, thus affecting the equilibrium of the inner ear structure & ossicular spatial relationships (Ash & Pinto, 1991; Buraa & Alazzawi, 2013) .
Active stability & movement are provided by the muscles of the jaw, the most important of which to consider in the development of & symptoms experienced through TMJD are the masseter, the pterygoids (lateral & medial) & the temporalis.
To get a more visual representation of the anatomy, click on the link below, which will take you to a slide show I found on SlideShare, by Martin Bush & was a useful revision tool.
Bush, M. Temporomandibular Joint. http://es.slideshare.net/bushmart/temporo-mandibular-joint
Indirectly, the relationship between the position of the TMJ (plus associated muscles) & the length/strength of the sub-occipital muscles influencing the subsequent joint positions of C1 & C2 is a very important factor when considering TMJD & the impact on posture (Urbanowicz, 1991; van Assche, 2006)
The key sub occipital muscles to be aware of in this respect are the rectus capitis posterior major & minor along with the obliquus capitis inferior & superior.
|
Muscle |
Origin |
Insertion |
|
Rectus capitis posterior minor |
Atlas (C1), posterior tubercle |
Below inferior nuchal line |
|
Rectus capitis posterior major |
Axis (C2) |
Inferior nuchal line |
|
Obliquus capitis superior |
Atlas (C1), lateral mass |
Inferior nuchal line |
|
Obliquus capitis inferior |
Axis (C2) |
Lateral mass of atlas (C1) |
Given the origins & insertions of these muscles, they can influence the relative positions of the C1 & C2. If either vertebrae is pulled out of position by pathological muscle tone, this will also affect the movements between the occiput & atlas (C0 & C1), atlas & axis (C1 & C2) as well as the other cervical joints, as the movements between them are not isolated or segmental; rather the movement of one joint entails movement in the adjacent joints.
Further stress on atlas position can occur in TMJD as the hyoid bone that attaches to the the jaw is also connected to the back of the skull in the region of the atlas. In addition, the hyoid is an attachment point for several of the small deep muscles of the neck & acts like a joiner’s spirit level contributing to the regulation of body alignment relative to the horizontal.
Therefore, mandibular displacement, will cause a displacement of the hyoid bone, which in turn will alter the resting tension of the myofascial chains that govern the static posture of the body through the laws of tensegrity.
It is then easy to trace an asymmetry from the cervical spine down, through a chain reaction, to other asymmetries throughout the rest of the skeleton as the body tries to compensate for a deviation away from a horizontal eye-line & a centralised position of the head’s mass (Fink et al, 2003).
Once the distribution of mass changes, stress on remote joints will also be redistributed creating abnormal patterns of load.
Such adaptations can increase pressure on the intervertebral discs, neural structures, blood vessels & organs, whilst optimal biomechanics of gravity-resisted tasks, like gait, can be completely altered (Rothbart, 2008).
If you consider the atlas alone, there are considered to be four variations of misalignment that can occur, each affecting the posture in different ways. These dysfunctions are well illustrated at Atlantotec’s website (www.atlantotec.com)
A parietal shift of the atlas, will result in a sideways tilt causing a scoliotic posture & a subsequent deviation of the posture from the symmetrical axis, having knock on effects on shoulder symmetry & pelvic tilt.
A rotation of the atlas on its horizontal axis is less likely to have major postural effects. Whilst it may potentially cause a rotation of the ribcage, thus influencing the pelvis, the more significant effect may be to exert pressure on the nerves, arteries & lymphatic ducts that surround the atlas.
Meanwhile, an atlas that becomes shifted dorsally (backwards) will contribute to an increased kyphosis & lumbar lordosis, whilst one shifted ventrally (forwards) will contribute to a loss of cervical &/or lumbar lordosis.
The C0-C1 joint also plays a major role in balance & proprioception, due to the extensive amount of neurological cross-linking & significant number of muscle spindles in the area, which provide considerable proprioceptive information.
As a starting point for studying TMJD, the relationship between the anatomy of the jaw, TMJ, hyoid bone, sub-occipital muscles & cervical spine is a good place to start to understand the importance of including this area in your musculoskeletal assessments & screening profiles.
In the next blog, I will start to look at more physiological influences that TMJD can have on performance capabilities of athletes, specifically in relation to skill acquisition, neuro-motor development & on the potential considerations in the concussed athlete.